Tackling the Challenges of Global Health
By Katherine Corley
Reporting Texas
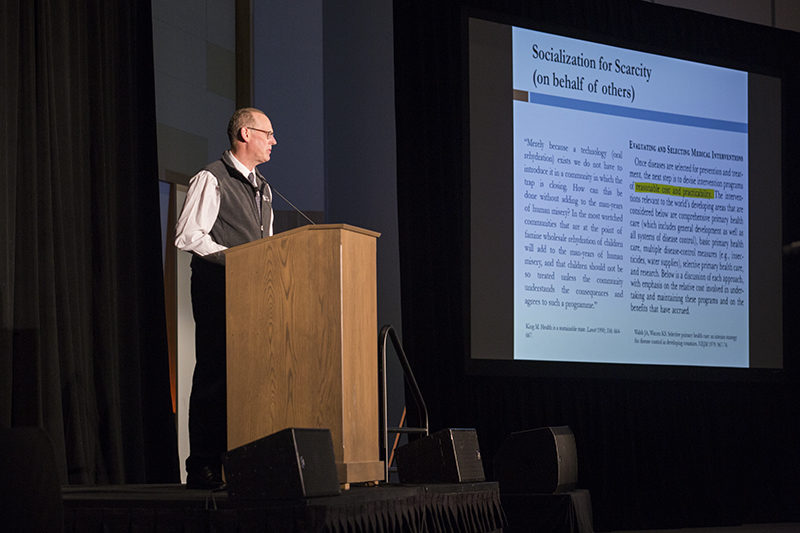
Dr. Paul Farmer discusses the research that went into his book “Reimagining Global Health: An Introduction” on April 15, 2019, at the AT&T Executive Education and Conference Center. Maria Toro/Reporting Texas
Dr. Paul Farmer is a widely recognized expert in the field of international health. He is co-founder of Partners in Health, a nonprofit organization that provides health care in developing countries. Farmer also serves as the chair of the department of global health and social medicine at Harvard Medical School and U.N. special adviser to the secretary-general for community-based medicine and lessons from Haiti. He spoke at the University of Texas at Austin on April 15 as part of the Joe Thorne Gilbert Lecture series. Before his lecture, Farmer sat for an interview with Katherine Corley of Reporting Texas. Excerpts:
On assisting vulnerable populations:
I could say, well, the best return on the dollar is girls’ education … I believe that’s true, right? … But [then] again, girls have to be healthy and protected. And boys too. I’m just saying this either-or logic has been the source of lots of problems in development. I could say, well, we really should start with primary care and strong community health worker programs. But if you ever are hit by a car, as I was in medical school, you’re going to hope there’s a trauma team. Or if you get cancer, you’re going to hope that was somebody’s priority … I do think we’ve learned lots about what a really good investment is, if your return is better health.
On the biggest challenge going forward:
Right now, [we’re] in this trap where we’re trying to choose between two or three or five good, necessary things. And we’re allowing them to compete with each other. So girls’ education should never be in competition with access to basic health care. Just like a tertiary hospital or trauma center shouldn’t be in competition with a community health system. But they are.
In fact, that leads to a lot of tribalism and infighting between the health and development folks. It’s counterproductive. And it turns our attention away from places where we could find resources. … After 30 years of pitting social and economic rights against other kinds of rights – I mean, not [Partners in Health], I hope we’re not doing that – or forgetting that health and education are indissociable, I think that’s something folks are willing to say: Well, we made a mistake, and we should never say one place to start is education versus basic safety nets.
On the most effective model for health care delivery in the U.S.:
Well, all these things I’m talking about: community health workers, more seamless coverage programs, especially for folks who are often in and out of emergency rooms. … [I’m saying] we need national safety nets. I’ll give an example. A lot of academic medical centers, or hospitals in general, have to make their emergency rooms open to all comers. Or they might not qualify for other kinds of federal assistance. I think it’s a very good idea. Does it lead to abuse of the emergency rooms? Well, I think it leads us to acknowledge we have been very abusive as a nation … we have a history of it, right? If people are obliged to go to an emergency room for care that might have been provided elsewhere, at least they have somewhere to go. So to me, that’s a safety net. It’s not a well-constructed safety net. That’s going to include things like childcare, leave for pregnancy, a whole suite of basic safety net services. I’m for them.